T Cell Therapy: A Revolutionary Approach to Cancer Treatment

T cell therapy
Over time, cancer treatment has changed dramatically, and immunotherapy has emerged as a ground-breaking strategy. T cell therapy, which uses the body's immune system to target and kill cancer cells, is one of the most promising developments. Some malignancies have responded remarkably well to this novel treatment, giving patients who would otherwise have few options hope.
What is T Cell Therapy?
T cell therapy involves modifying a patient’s own immune cells (T cells) to enhance their ability to recognize and attack cancer. There are two primary types:
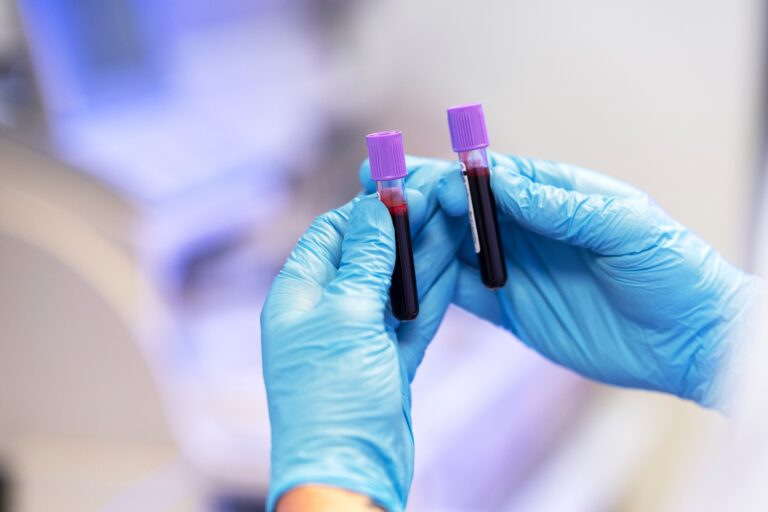
- CAR T Cell Therapy (Chimeric Antigen Receptor T Cell Therapy) – Scientists extract T cells from a patient’s blood, genetically engineer them to produce special receptors (CARs) that target cancer-specific proteins, and then infuse them back into the patient.
- TIL Therapy (Tumor-Infiltrating Lymphocyte Therapy) – Immune cells that have already penetrated tumors are extracted, multiplied in a lab, and reintroduced into the patient to boost the anti-cancer response.
How Does T Cell Therapy Work?
The first step in T cell therapy is to extract the patient's own T cells from their blood. Then, in the lab, these cells are genetically altered to produce specialized receptors (CARs) that can recognize and attach to antigens unique to cancer, especially in CAR T treatment. To provide a strong therapeutic dose, the T cells are cultivated in huge numbers after they have been modified. The improved T cells are then reintroduced into the patient's circulation, where they aggressively hunt down and eliminate cancer cells, utilizing the body's own defenses to eradicate specific tumors.
Successes in Cancer Treatment
T cell therapy has shown remarkable success in treating aggressive blood cancers, including acute lymphoblastic leukemia (ALL), non-Hodgkin lymphoma, and multiple myeloma, with some patients achieving long-term remission even after other treatments failed. While CAR T-cell therapy has revolutionized care for these malignancies, researchers are now expanding its potential to combat solid tumors—such as breast, lung, and ovarian cancers—where challenges like the tumor microenvironment have previously limited effectiveness. Ongoing clinical trials aim to unlock broader applications, bringing hope to more cancer patients worldwide.
Challenges and Side Effects
Despite its promise, T cell therapy has limitations:
- Cytokine Release Syndrome (CRS): An overactive immune response causing fever, low blood pressure, and organ dysfunction.
- Neurotoxicity: Some patients experience confusion or seizures.
- High Costs: The personalized nature of the therapy makes it expensive.
- Limited Efficacy in Solid Tumors: The tumor microenvironment can suppress T cell activity.
The Future of T Cell Therapy
The future of T cell therapy looks promising as researchers work to enhance its precision, broaden its applications, and improve accessibility. Scientists are focused on refining targeting mechanisms to minimize side effects while expanding treatment options to include more cancer types beyond blood malignancies. A particularly exciting development is the creation of T"off-the-shelf" CAR T cells derived from healthy donors, which could significantly lower costs, reduce manufacturing delays, and make this life-saving therapy available to more patients worldwide. These advancements could cement T cell therapy as a cornerstone of modern oncology.
T cell therapy represents a major leap forward in cancer treatment, offering new hope where traditional therapies fail. While challenges remain, continued advancements could make it a cornerstone of oncology, transforming the way we fight cancer. As clinical trials progress, this revolutionary approach may soon become a standard treatment, bringing us closer to a future where even the most aggressive cancers can be effectively controlled or cured.